By guest author: Devin Fisher, M.S., CCC-SLP
Suggestions for Communicating with People with Aphasia
- Continue to treat people with aphasia as the mature adults that they are.
- Regard people with aphasia as communicating individuals even though they may not understand what you are saying. Don’t bombard them with too much speech or too many people talking.
- Do not talk about people with aphasia in their presence, even if they appear comatose or show no indication of comprehension of speech. Don’t assume that because they’re not reacting or because they don’t speak that they do not understand.
- On the other hand, don’t assume that people with aphasia do understand.
- Remember that people with aphasia get cues from the environment, gestures, and facial expressions. People with aphasia’s ability to grasp the meaning of what is said may be due to these situational cues rather than to an understanding of the actual words.
- When speaking to people with aphasia, stand on the uninvolved side so you will be within his or her visual field.
- Keep communication short and simple and accompany it with gestures.
Speak in a natural voice. Unless you know there is a hearing loss, don’t assume that by speaking louder people with aphasia will understand better. - If people with aphasia’s “yes” and “no” responses are reliable, ask direct questions requiring these responses rather than ones necessitating a complex answer.
- Allow people with aphasia to attempt to speak.
- Where there is a word-finding problem, give people with aphasia the opportunity to recall the word themselves; supply a word only when you see that people with aphasia are becoming frustrated and/or ask for assistance
- When people with aphasia become frustrated at the inability to recall a word and you know the word he or she is searching for, you may help by setting up an automatic speech situation such as sentence completion. If you say, “I want a drink of ____________” and then pause, the person with aphasia may be able to fill in the word.
- Encourage the use of greetings and other verbal social amenities. Not only do they serve as models for the person with aphasia to copy, but also they are typically automatic speech responses that he or she may be able to make.
- Don’t correct the person with aphasia’s errors. Rather, restate what you think he or she was saying. This will help establish whether you understand what was said and give the person with aphasia an opportunity to hear the correct version.
- Be alert for delayed responses in people with aphasia who can respond if given enough time to do so.
- Give increased time to respond; don’t push responses.
- Repeat questions; verbalize in a different way.
- Focus on abilities versus disabilities.
- Push self-care and tangible, achievable goals.
- Focus on language for people with aphasia’s immediate, specific needs (e.g., help the person with aphasia to ask for the bedpan rather than to name body parts).
- Treat people like the adults they are.
- Be natural and encourage participation whenever possible.
- Keep the person with aphasia in a social world to help prevent withdrawal and depression.
- Use routine activities for speaking and reinforcing therapy techniques.
- Let the person with aphasia ask for what he or she wants.
- Provide the names of the objects in use.
- Should the person with aphasia indicate a desire to be helped with a word, pronounce it slowly and distinctly.
- Anticipating what the person with aphasia is trying to say by voicing it for them may impede progress in speech and language development. Always encourage people with aphasia to speak and do for themselves.
- If the person with aphasia swears or voices emotional utterances, avoid any show of disapproval. To express annoyance or reprove a person with aphasia may inhibit attempts at communication.
Let people with aphasia express themselves on their own speech and language level. Exert every effort to understand what the person with aphasia is trying to tell you. - Don’t force speech when the person with aphasia is fatigued.
- The person with aphasia should not be made to perform speech or language activities for an audience or group of visitors.
- Stimulate a person with aphasia with various mediums for language (conversation, music, TV, radio, Internet, podcasts).
The above suggestions are general in nature and meant to apply to the widest breadth of caregivers caring and living with individuals with aphasia. Not all of these suggestions may apply to your situation. However, I hope these suggestions help to guide you in the right direction and facilitate a better relationship with you and your loved one(s).
If you enjoyed these suggestions, you may appreciate other recommendations and resources at speakupthinkup.com.
About the author:
Hi, my name is Devin! I’m a practicing speech-language pathologist in Las Vegas, Nevada. I care deeply about helping others and hope to help many people locally and abroad. I started Speak Up, Think Up! to get more resources into the hands of those that need them.
About Contributor
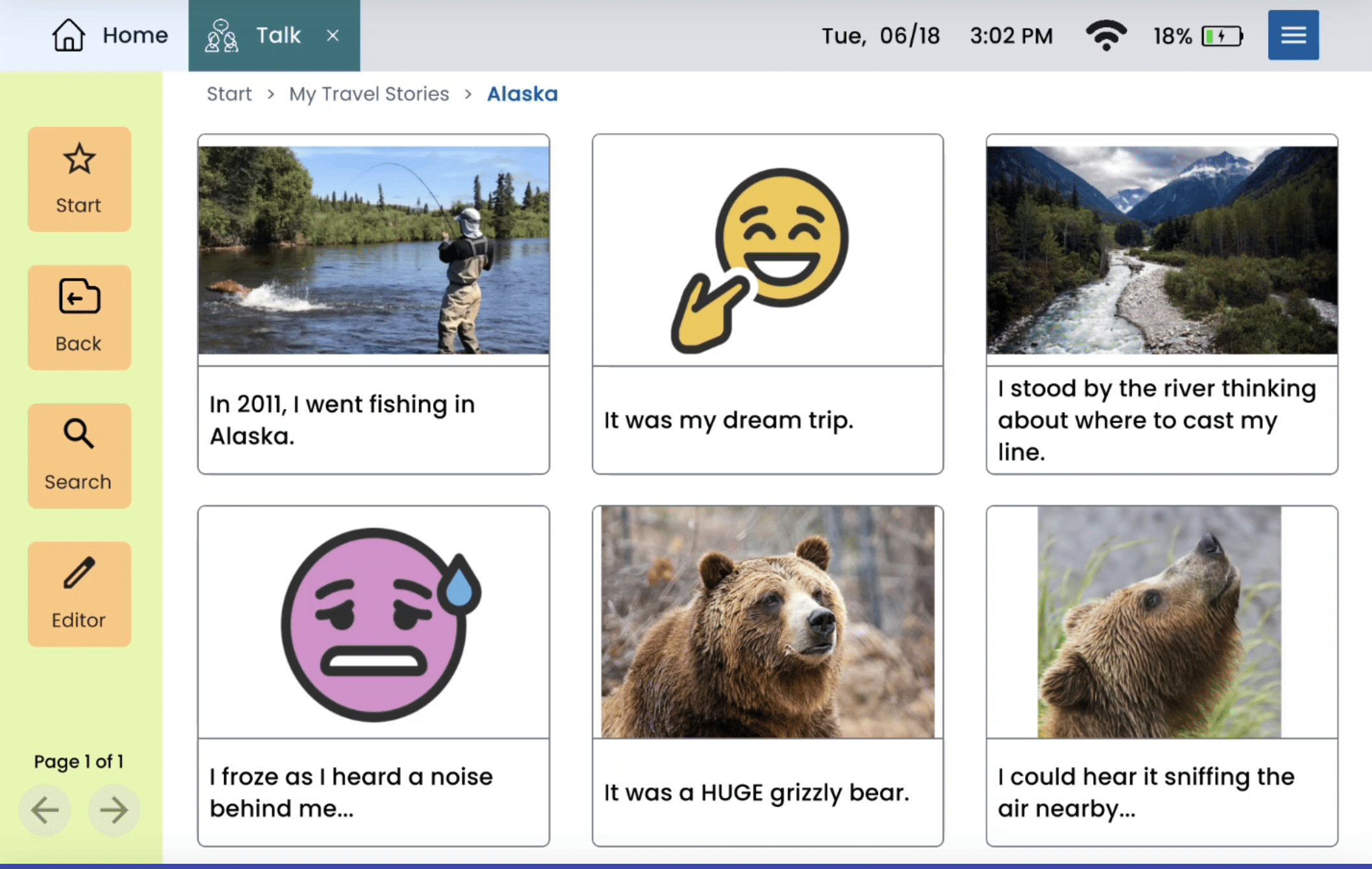
Lingraphica helps people with speech and language impairments improve their communication, speech, and quality of life. Try a Lingraphica AAC device for free.